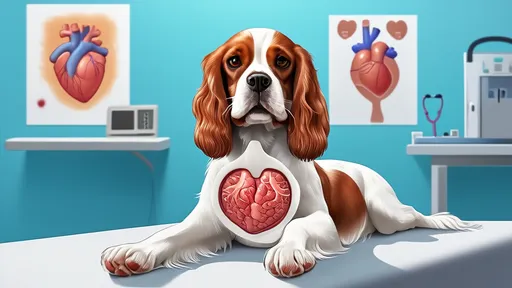
In the world of purebred dogs, few conditions are as intimately linked to a specific breed as mitral valve disease is to the Cavalier King Charles Spaniel. For owners and breeders of these affectionate companions, the term MVD is not merely a veterinary acronym; it is a specter that looms over the breed's future, a central concern in every conversation about health and longevity. The connection is so profound that to speak of one is to inevitably invoke the other, creating a narrative of both deep affection and profound concern within the community.
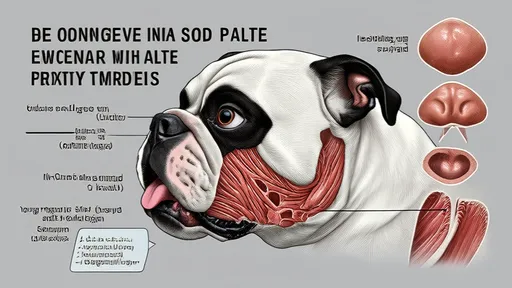
The mitral valve itself is a small but critical structure within the heart, acting as a one-way gate between the left atrium and the left ventricle. Its proper function is essential for efficient blood flow. In a healthy heart, the valve's two leaflets open fully to allow blood to pass into the main pumping chamber and then snap shut with precision to prevent any backward leakage. In Cavaliers affected by MVD, this elegant system breaks down. The valve leaflets, and the cords that anchor them, gradually thicken and become misshapen. They no longer form a perfect seal. With each powerful contraction of the ventricle, a portion of oxygenated blood is forced backward, or regurgitated, into the atrium. This is the hallmark murmur that a veterinarian hears through a stethoscope—the sound of turbulence where there should be silence.
This initial leak may seem insignificant, a mere whisper of a problem, but its consequences are cumulative and devastating. The heart, a remarkably adaptive organ, compensates for this inefficiency. It dilates, enlarging its chambers to handle the increased volume of blood. It beats faster and more forcefully. For a time, these compensatory mechanisms work, and the dog shows no outward signs of illness. This is the insidious nature of early-stage MVD; it is a silent thief, stealing cardiac function long before any symptoms alert the owner. However, this state of compensation is unsustainable. The heart muscle, overworked and stretched beyond its limits, begins to fail. The pressure buildup from the regurgitated blood eventually causes fluid to leak into the lung tissue, a condition known as congestive heart failure. It is at this point that the dog's body can no longer mask the problem, and the clinical signs become painfully apparent.
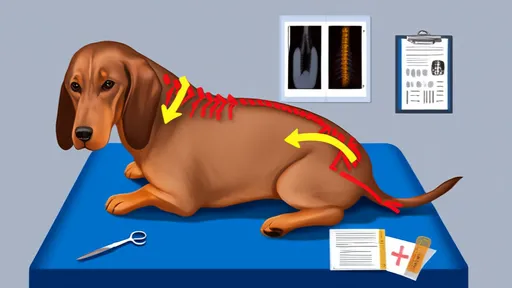
Recognizing the progression of MVD is paramount. In the earliest stages, there are truly no visible symptoms. The only indicator is that soft murmur, often discovered during a routine check-up. As the disease advances to moderate stages, the first subtle signs might emerge. A once-energetic dog may tire more easily on walks, perhaps needing to stop and catch its breath sooner than expected. They might cough occasionally, particularly at night or upon waking, a result of slight fluid accumulation. Many owners dismiss these signs as mere aging or a minor throat irritation. The transition to severe, overt congestive heart failure is often dramatic. The cough becomes persistent and hacking. Breathing becomes labored, rapid, and shallow, even at rest. The dog may struggle to get comfortable, restlessly pacing or sitting with elbows splayed to try and expand its chest. A profound lethargy sets in, and fainting spells can occur due to inadequate blood flow to the brain. The appearance of these symptoms constitutes a medical emergency.
Given the genetic underpinnings of the disease, diagnosis is not a single event but an ongoing process of monitoring. Auscultation—listening to the heart with a stethoscope—is the first and most crucial line of defense. Veterinarians will grade the intensity of the murmur on a scale of one to six. A murmur that increases in grade over successive visits confirms the disease is progressing. However, the murmur alone does not paint the full picture. An echocardiogram, an ultrasound of the heart, is the gold standard for diagnosis. This non-invasive procedure allows a cardiologist to visualize the leaking valve, measure the degree of regurgitation, and assess the size and function of the heart chambers. Chest X-rays are invaluable for evaluating the overall size of the heart and, most importantly, for detecting the pulmonary edema (fluid in the lungs) that signifies the onset of heart failure. Together, these tools create a comprehensive picture of the disease's stage and severity, guiding every treatment decision.
While there is no cure for MVD, treatment strategies have evolved significantly, focused on managing symptoms, improving quality of life, and prolonging survival. The approach is tailored to the stage of the disease. For early-stage MVD, the approach was once a watchful waiting, but a groundbreaking study, the EPIC study, has changed standard practice. It found that starting a medication called pimobendan early, even before the onset of heart failure, can significantly delay the onset of congestive symptoms and extend a dog's life. This has been a revolutionary shift in management. Once heart failure begins, the therapeutic arsenal expands. Diuretics like furosemide are the cornerstone of treatment, aggressively pulling excess fluid from the lungs to ease breathing. ACE inhibitors help dilate blood vessels, reducing the workload on the heart and mitigating the harmful hormonal activation that heart failure triggers. Pimobendan remains crucial for its dual action of strengthening the heart's contractions while also dilating vessels.
The grim reality is that MVD is a progressive and ultimately fatal disease. The prognosis is tightly linked to the stage at which it is identified and treated. A dog with a mild murmur may live a normal lifespan for many years. Once the heart begins to enlarge noticeably on an echocardiogram, the clock ticks faster. The onset of congestive heart failure marks a critical turning point; with aggressive and dedicated treatment, many dogs can still enjoy a good quality of life for another year or two, sometimes longer. The final stages of the disease are managed with palliative care, focusing on comfort until a quality of life is no longer sustainable. This heartbreak is what drives the community's intense focus on prevention, which lies almost exclusively in the realm of responsible breeding.
The heritability of MVD in Cavaliers is one of the most well-documented in all of veterinary medicine. It is a polygenic disease, meaning multiple genes are involved, making it a complex challenge to eradicate. In response, kennel clubs and breed organizations worldwide have established stringent protocols. The most widely adopted is the heart scheme pioneered by the UK and followed by many other countries. It recommends that no Cavalier be bred from until they are at least 2.5 years old and have been certified by a specialist cardiologist to be free of a murmur. Even more robust protocols advise only breeding from dogs that are still clear at five years of age, as the disease's late onset means a clear exam at 2.5 is not a lifetime guarantee. The goal is to slowly increase the age of onset in the gene pool with each generation, pushing the disease later and later in life until it no longer impacts a dog's natural lifespan. This is a slow, generational effort requiring immense commitment from breeders.
For an owner, receiving a diagnosis of MVD can feel overwhelming. The journey from that first faint murmur to the final goodbye is a path paved with regular veterinary visits, daily medications, and constant vigilance. It requires learning to recognize the subtle signs of good and bad days. Yet, it is also a journey defined by profound love and companionship. Modern medicine provides powerful tools to manage this disease, offering not just additional time, but good quality time. The bond between an owner and a Cavalier navigating heart disease is deep, forged in the shared daily routine of care. The goal is never to cure the incurable, but to ensure that every day is filled with comfort, affection, and the simple joys of being a dog—a chase of a ball in the yard, a cozy nap in a sunbeam, a gentle nudge of a nose. The story of the Cavalier King Charles Spaniel and MVD is one of challenge, but it is ultimately a story of resilience, dedication, and the enduring strength of the human-animal bond.
By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025
By /Aug 20, 2025
By /Aug 20, 2025
By /Aug 20, 2025
By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025

By /Aug 20, 2025